Patients visit my proctology clinic, complaining of symptoms such as bleeding, pain, discomfort, and itching in the perianal region. In most cases, such symptoms are indicative of such conditions as "hemorrhoids (piles)," "anal fissure," or "anal fistula." However, they may be symptomatic of any of the following diseases other than hemorrhoids: perianal dermatitis in patients with perianal discomfort or itching, and pudendal neuralgia in patients with pain. This is an example of a case where a patient who had undergone surgery for internal hemorrhoids visited my clinic, complaining of persistent postoperative pain. Since the patient also had pudendal neuralgia, the patient’s condition was aggravated by comorbid genital neuralgia and postoperative pain. It is important to properly identify the cause of pain or discomfort after careful consideration as to whether the cause is hemorrhoids and to provide appropriate treatment, not simply judging it as hemorrhoids.
Patients are usually shocked by anal bleeding, and anal bleeding is not always due to hemorrhoids. When you visit the hospital, the color and appearance of the blood from anal bleeding will be asked first. If the blood color is black, it means the bleeding from the upper gastrointestinal tract, such as the stomach and esophagus. If the blood color is reddish, it means it is from the large intestine. Depending on the case, appropriate tests and treatment will be given. In most cases, the blood from anal bleeding is bright red (fresh blood). This is bleeding from the anus, the rectum close to the anus, sigmoid colon or such, which may be due to cancer around the anus, and tests for cancer must be performed as soon as possible. Although rare, there are some patients presenting with severe bleeding due to ruptured internal hemorrhoids. In such cases, immediate surgical procedures must be performed on that day and, thus, it is essential for such patients to visit a hospital as soon as they become aware of the problem.

In the case of anal bleeding, the possibility of cancer must be suspected. The treatment of hemorrhoids and of cancer are different fundamentally. In the case of cancer, immediate and intensive cancer treatment must be taken. If the possibility of cancer is suspected in a patient presenting with anal bleeding and if it can be scheduled, an endoscopy will be performed on the day to check for the absence/presence of any lesion in the large intestine. Such patients are hoping that the diagnosis will be hemorrhoids, not colorectal cancer. It is the responsibility of the doctors to suspect cancer first and then rule out its possibility without hastily making a diagnosis of hemorrhoids.
Patients who visit a clinic or hospital presenting with anal bleeding and pain are often suffering from any of the following three major diseases: "hemorrhoids (piles)," "anal fissure," and "anal fistula." There are however a number of other possible diseases such as "perianal dermatitis" and "pudendal neuralgia." With regard to "pudendal neuralgia" in particular, persistent pain may continue. There are some patients suffering from persistent pain even after surgery and treatment for "hemorrhoids (piles)." In such patients, a surgical procedure might have increased "pudendal neuralgia." Since postoperative pain may exacerbate neuralgia, appropriate treatment must be determined after careful consideration.
A specialist qualified by the Japan Society of Coloproctology, whether in the field of proctology or colorectal surgery, is a physician who has completed a specialized training course, and thus it is recommended to visit a clinic or hospital where such a specialist is available. If there is no specialist available at a nearby clinic or hospital, it is recommended to first consult with your family doctor to be referred to a specialist. In recent years, an increasing number of people have been collecting information on such specialists using the Internet. However, you must keep in mind that not all of the information on the Internet is reliable, so you must collect information with much caution. If you have an acquaintance, especially a healthcare professional who has some knowledge of or experience in your problem, his or her advice may be helpful.
The advantage of clinics over large hospitals is their flexibility. When no other person is waiting in a clinic, it takes less than one hour for a patient to complete the first visit, including examinations such as endoscopy, because only several minutes are required for such an examination. Even if the clinic is a little crowded, it will take only 2 hours to complete the visit. Our clinic has an in-house pharmacy at which we dispense prescription drugs. The costs incurred are inclusive, so if they appear to be high, in reality they are not so, because the patient will not have to visit a pharmacy outside of our clinic to purchase medications. If a patient makes a first visit to our clinic and is prescribed drugs for constipation or hemorrhoids at our clinic, the patient will have to pay 10% (about 760 yen) or 30% (about 2300 yen) of all expenses depending on their health insurance coverage. Even if an endoscopy (including sigmoidoscopy) is performed on a patient presenting with bleeding, the patient’s self-payment will be about 1400 yen (10%) or 4200 yen (30%). With such amount of money, a correct diagnosis of hemorrhoids or colorectal cancer can be established with a considerably high probability. Such a cost is acceptable. If you are concerned about perianal conditions, visit a clinic as soon as possible “before it is too late for treatment.”
Goligher’s classification indicates the degrees of symptoms (prolapse) of hemorrhoids (piles). The degrees of hemorrhoids are largely classified into the following 4 grades: grade 1, bleeding but no prolapse; grade 2, prolapse through the anus on straining but reduced spontaneously; grade 3, prolapse through the anus on straining or exertion and require manual replacement into the anal canal; and grade 4, prolapse stays out at all times and is irreducible. Surgery is required for Grade 3 and 4 hemorrhoids. The standard surgical procedure for hemorrhoids is ligation and excision (LE). Currently, methods to cure internal hemorrhoids by injection have been widely used, and options such as day surgery have also expanded. Regarding cancer treatment, approaches that focus on cure of the disease are required and deviation from treatment guidelines may place patients at risk; however, proctology treatment is basically to remove symptoms patients are suffering from. At our clinic, we provide a patient with a medical diagnosis and determine the appropriate treatment method after consultation with the patient in consideration of the patient's daily life including work.
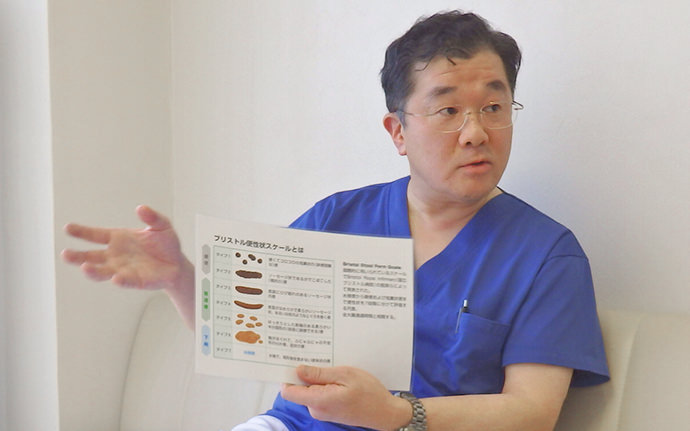
There are many patients who visit our clinic with the chief complaint of "constipation"; however, the degrees of constipation differ according to individual patients’ expectancies. Some patients regard “having trouble at the time of bowel movement” as constipation, while others regard "less frequent bowel movements" as constipation. It is important for the physician to ask the patient about his/her daily and weekly frequencies of bowel movements, and the form and color of stools. At our clinic, the frequency of bowel movements is investigated and the contents of stools are checked using pictures of stools as samples for the patient.
Many of the patients complaining of constipation have been taking irritant laxatives available as over-the-counter (OTC) medications over the long term, which is one of the factors associated with difficult defecation/abnormal feces. For these patients, we prescribe weak irritant laxatives with the aim of gradually reducing dependence on such OTC laxatives and of alleviating symptoms of constipation.
According to the conventional criteria, 3 or more bowel movements per week and bowel movements up to 3 times per day are defined as normal weekly and daily frequencies. However, in my opinion, a bowel movement once in the morning before breakfast is physiologically healthy. In the animal world, bowel movements occur at dawn to evacuate the bowels before feeding starts. In my opinion, it is the same for humans. In my opinion, it is ideal to empty your bowels once in the morning and not to have another bowel movement until the next morning. Some people have bowel movements after each meal; men, in particular, have frequent bowel movements. This is called the gastrocolic reflex. The gastrocolic reflex itself is not indicative of a problem; however, in terms of bowel movement control, the recommended frequency is once a day. Basically, lifestyle guidance and drugs to control stool consistency and bowel peristalsis will be used to alleviate constipation. However, if you can form the habit of a bowel movement once every morning regardless of whether you currently have frequent or infrequent bowel movements, you will be able to pass surprisingly good stools.

Fiber intake is recommended for some patients with constipation but this does not always alleviate constipation. Fiber intake is very effective in patients with constipation despite no problem with the transit time of food through the large intestine, while it is not effective in patients with constipation whose intestinal transit time is long due to intestinal hypomotility. The presence/absence of such intestinal problems must be checked. Eating soybeans is recommended for patients in whom fiber intake is effective against constipation. Natto (fermented soybeans) and soymilk are also effective. Raw vegetables are not a main source of fiber. For patients with separate, hard lumpy stools, a magnesium preparation should be administered to soften stools. Such patients must also pay attention to how to drink adequate fluid. If a lot of cold water is drunk at once, most of it will soon be excreted in urine or sweat. It is therefore recommended that an extra 500 mL or more of room temperature water be drunk over the period of one day.